
Back Pain Treatment Home » Alternative Treatments » Short Term Treatments for Back Pain

Non-narcotic analgesics such as Non-steroidal Anti-inflammatory Drugs (NSAIDs) or Acetaminophen (Tylenol) can help control mild to moderate pain levels, especially pain from musculoskeletal problems such as muscle or joint pain. NSAIDs include naproxen, ibuprofen, diclofenac, etc and come in over the counter or prescription strengths. NSAIDs can lower inflammation as well as reduce pain. NSAIDs can decrease blood flow to the kidney and can result in gastrointestinal bleeding. It is important to take NSAIDs with food and stay hydrated as these medications may cause stomach ulcers and gastrointestinal bleeding and kidney injury. Non-narcotic analgesics include Acetaminophen (Tylenol) do not have the same risks as NSAIDs but can cause liver damage above 4000 mg per day. It is well advised not to take more than 3000 mg per day and not to drink any alcohol with Acetaminophen.
Muscle relaxants, such as Baclofen or Tizanidine help reduce back pain due to muscle spasm. Possible side effects of muscle relaxants include sleepiness or fatigue. A compounded cream containing muscle relaxants can help reduce pain due to muscle spasm without the fatigue and sedation of the oral route. Compounded creams are usually applied two to three times per day to the skin overlying the painful area. Multiple medications such as NSAIDS or local anesthetics can be added to a compounded cream in addition to a muscle relaxant to maximize the pain relief of the medications while minimizing side effects. Insurance does not always cover the compounded cream and sometimes a rash may develop from it.
It has long been known that certain antidepressants, most notably those that increase norepinephrine help to control nerve related pain by increasing the signals from the brain that quiet nerve impulses. Tricyclic antidepressants (TCA’s) such as Amitriptyline or Nortriptyline have been prescribed for chronic pain for many years, but a newer class of antidepressants, that increase Serotonin and Norepinephrine (SNRI’s), can lower pain due to chronic conditions such as arthritis, fibromyalgia, diabetic neuropathy with fewer side effects. Side effects, may include sexual dysfunction, nausea, and even possible suicidal ideation, so must be monitored by your physician.
Opioids are a last resort medication as there is little evidence that opioids improve function when prescribed for chronic, noncancer pain. Theories as to why opioids do not help in these circumstances include that the receptors that opioids work at become less sensitive or even fewer in number when opioids are taken orally or that the opioids themselves can cause increased sensitivity to pain (hyperalgesia). In either case, chronic pain may worsen as a result of opioid use.
Side effects of opioids include respiratory depression/death, slower thinking, constipation, lower testosterone leading to depression and impotency, as well as dependency (withdrawal symptoms if the opioid is stopped: anxiety, abdominal cramping, diarrhea, sweating and sleeplessness:), or addiction (compulsive use despite harm). For these reasons, opioids are rarely prescribed and if they are prescribed, it is at the lowest dose possible to prevent accidental overdose and fatalities. You would only be prescribed an opioid after: screening for addiction risk, a long discussion of risks/benefits, a discussion with your primary care/referring physician, and your informed consent. You would also be monitored at least monthly with in person visits for evaluation of function, side effects, proper use, and psychological dependency. Urine toxicology screens and review of all controlled medications you have been prescribed at each visit is a standard of care for any patient being prescribed opioids. Sometimes, we request a friend or family member who knows you well to come to an appointment to provide an objective opinion as to how the medication is affecting you.
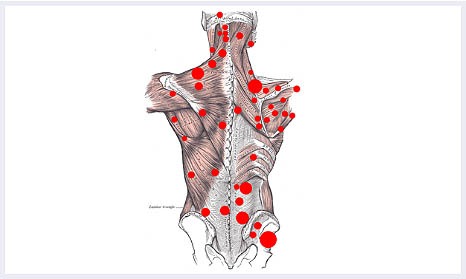

When trigger points are firmly pressed, the entire muscle can twitch or spring into spasm. Trigger points are often located in the neck, back or shoulder muscles, and can cause pain in all the muscles close by. Trigger points are diagnosed by examining signs, symptoms, pain patterns and manual palpation.
Trigger points can appear in many myofascial structures, including muscles, tendons, ligaments, skin, joint capsule, periosteal, and scar tissue. They can be caused by acute or chronic muscle overload, activation by other trigger points, disease, psychological distress, direct trauma to the region, infections or simply by pain nearby.
Treatment of trigger points include ultrasound, electrostimulation, ischemic compression, injection, and alternative therapies like massage, acupuncture. Injections provide more immediate relief, and can be effective when other methods fail. Various injections can be used, including saline, local anesthetics such as lidocaine, steroids, and Botox).
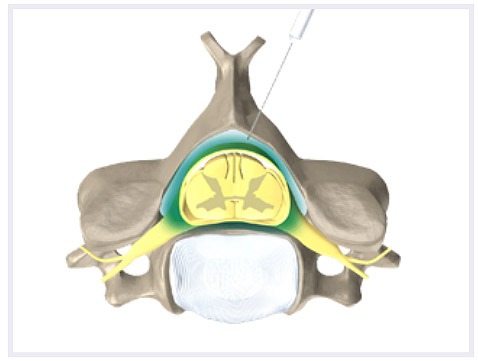
This type of injection is normally considered after nonsteroidal anti-inflammatory drugs and/or physical therapy have failed to provide adequate pain relief. Epidural Injections have been proven to be effective in relieving pain. For those who receive the injection within three to six months from the onset of pain, response rates can be as high as 70-90%. This response rate may lower for patients who have had prolonged pain. Other factors associated with a decreased response include age over 60 years, smoking, and a history of back surgery.
Repetition of an injection depends on the response to the treatment. For acute radicular pain symptoms, 3-4 Epidural Injections may be performed in total (usually one injection every 3-4 weeks). Complications from Epidural Steroid Injections are extremely rare but include headache, nerve injury and infection. Side effects may include a temporary elevation in blood sugar and fluid retention. More commonly, soreness at the injection site or a temporary increase in pain symptoms may be noted after the injection for a few days.
Facet joint injections and medial branch blocks are performed to diagnose and treat back pain that comes from the spinal facet joints. Facet joint pain is usually pain in the middle of the spine that can radiate down the legs to the knees, and sometimes to the calves (or radiate from the neck to the shoulders and upper back). Facet back pain is usually worse when arching the back or twisting the spine.
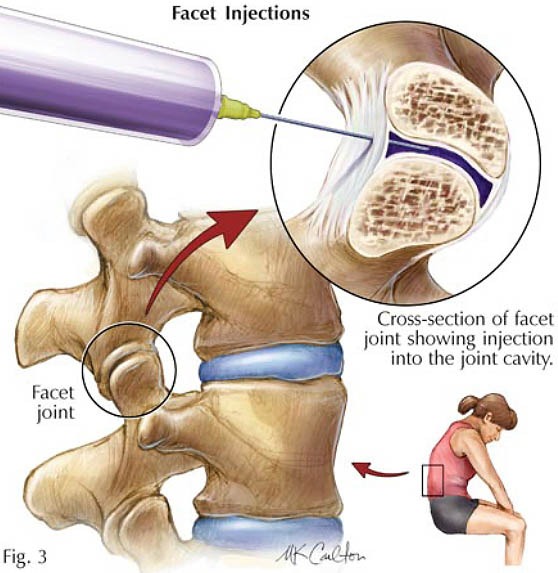
A facet joint injection involves placing the local anesthetic in the facet joint itself; whereas, a medial branch block involves depositing local anesthetic at the small, medial nerves to temporarily interrupt the transmission of pain signals sent from the facet joints to the spinal cord. A small dose of corticosteroid is usually mixed with the local anesthetic to provide for more long-term relief than with the local anesthetic alone. Both the facet joint injection and medial branch block are done with fluoroscopy (XRay machine) to allow precise placement of the needle.
Temporary pain relief from the local anesthetic should be experienced within 30 minutes of the procedure and often much sooner. The steroid effect may take several days to experience but can provide many weeks of back pain relief. There may be a couple of days after the procedure in which there is some increased soreness from the needle placement.
Risks of the procedure are extremely low, but include bleeding, infection, and nerve injury. You should contact your physician should you experience redness or heat at the site of the injection or if you feel significantly more back pain or feel unwell.
The facet joint injection and medial branch blocks should provide more than 50% pain relief from facet joint pain. If the blocks yield only a short duration of significant pain relief, a radiofrequency lesioning procedure of the medial branch nerves can provide as long as 9 months of pain relief should be considered.